Denosumab
Denosumab treats osteoporosis and can be used to prevent fractures from certain types of cancers that have spread to the bone. Before you have any dental work, tell your dentist you receive this drug.
Denosumab Overview
Denosumab is a prescription medication used to treat osteoporosis in postmenopausal women and men who are at an increased risk for a bone fracture. Denosumab is used to treat bone loss in men and women undergoing treatment for certain types of cancer.
Denosumab is also used to prevent fractures, spinal cord compression, or the need for radiation or surgery to the bone in those with multiple myeloma or those with solid tumors that have spread to the bone. It is also approved to treat giant cell tumor of the bone that cannot be treated with surgery. Denosumab is also used to treat high levels of calcium due to cancer that has not been successfully treated with bisphosphonate therapy.
Denosumab belongs to a group of drugs called RANK ligand inhibitors. These work by decreasing the breakdown of bone and increasing bone strength and thickness.
This medication comes in an injectable form to be given under the skin (subcutaneously) and is given anywhere from once a month to once every 6 months, depending on the condition being treated.
Common side effects of denosumab include red, dry, and itchy skin, back pain, and headache.
How was your experience with Denosumab?
Denosumab Cautionary Labels
Uses of Denosumab
Denosumab is used to treat:
- osteoporosis in postmenopausal women and men who are at an increased risk for a bone fracture
- bone loss in men with prostate cancer and women with breast cancer receiving certain treatments
- prevent fractures, spinal cord compression, or the need for radiation or surgery to the bone in those with multiple myeloma or those with solid tumors that have spread to the bone
- giant cell tumor of the bone that cannot be treated surgically. Denosumab is also used to treat high levels of calcium due to cancer that has not been successfully treated with bisphosphonate therapy.
This medication may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Denosumab Brand Names
Denosumab Drug Class
Denosumab is part of the drug class:
Side Effects of Denosumab
Serious side effects have been reported with denosumab. See the "Drug Precautions" section.
Common side effects of denosumab include the following:
- red, dry, itchy skin
- back pain
- nausea
- headache
- pain in arms or legs
- joint pain
- muscle pain
- fatigue
- increase in cholesterol
- upper respiratory tract infections
- decreased appetite
- swelling in the hands or feet
This is not a complete list of denosumab side effects. Ask your doctor or pharmacist for more information.
Tell your doctor if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Denosumab Interactions
No drug interactions have been determined by the manufacturer. However, you should tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements. Not all drug interactions are known or reported and new drug interactions are continually being reported.
Denosumab Precautions
Serious side effects have been reported with denosumab including the following:
- Anaphylaxis. Anaphylaxis is a severe, life-threatening allergic reaction. Seek immediate medical attention if you experience any of the following symptoms: swelling of the lips, tongue, or throat, difficulty breathing, dizziness, or itching.
- Hypocalcemia. Hypocalcemia refers to low levels of calcium in the blood. Tell your doctor if you experience any of the following symptoms of hypocalcemia: muscle stiffness or spasms, dizziness, or numbness in the fingers. Your doctor may check your calcium level in your blood before you use denosumab to make sure it is not too low. Your doctor should also instruct you to take calcium and vitamin D supplements during treatment to make sure your calcium does not get too low.
- Osteonecrosis of the jaw. Osteonecrosis is a serious bone disease that can degrade bone and limit its function. It typically occurs after tooth extraction or local infection. You should have a dental exam before you start treatment with denosumab.
- Fractures of the femur. While denosumab is intended to prevent fractures, patients using the drug have experienced fractures. Tell your doctor if you notice any new thigh, hip, or groin pain.
- Infection. Tell your doctor if you notice any signs of infection such as a cough, runny nose, sore throat, or fever.
- Skin reactions. Tell your doctor if you develop a rash or develop itching, burning, or redness of the skin.
- Bone, joint, and muscle pain. Stop taking denosumab and tell your doctor if you experience pain in the joints, or deeper in the muscle or bone.
- Decreased bone remodeling. It is not known if denosumab use over a long period of time slows the healing of broken bones.
- Multiple vertebral fractures (MVF) following treatment discontinuation. After treatment denosumab is stopped there may be an increased risk of having broken bones in the spine especially in patients who have had a fracture or who have had osteoporosis. It is not recommended to interrupt denosumab therapy without your doctor's advice.
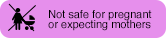
- Harm to your unborn baby. Women who are able to become pregnant are recommended to use effective contraception during therapy, and for at some time after the last dose of Xgeva. Your doctor will tell you how long after your last dose you will have to use effective contraception.
Do not use denosumab if you:
- are allergic to denosumab or any of its ingredients
- have an infection
- are pregnant
- have low calcium levels
Denosumab Food Interactions
Medications can interact with certain foods. In some cases, this may be harmful and your doctor may advise you to avoid certain foods. In the case of denosumab, there are no specific foods you must exclude from your diet when receiving this medication.
Inform MD
Before taking denosumab, tell your doctor about all of your medical conditions. Especially tell your doctor if you:
- Are allergic to denosumab or any of its ingredients
- Have had recent dental work, or plan to have dental work or a tooth extraction in the future
- Have been told you have low calcium levels in your blood
- Have kidney problems
- Are unable to take calcium or vitamin D supplements
- Have been told you have trouble absorbing vitamins or minerals in your stomach or intestines
- Are taking another medicine that contains denosumab. Denosumab is marketed as Xgeva and Prolia, and patients receiving either one of these medications should not receive the other.
- Have an active infection
- Have had thyroid or parathyroid (glands located in your neck) surgery
- Are pregnant or are plan to become pregnant
- Are breastfeeding or plan to breastfeed
- Tell your dentist that you are receiving denosumab before you have dental work done
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
Denosumab and Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant.
The FDA categorizes medications based on safety for use during pregnancy. Five categories - A, B, C, D, and X, are used to classify possible risks of an unborn baby when a medication is taken during pregnancy.
Denosumab falls into category X. It has been shown that women taking denosumab during pregnancy may have babies born with problems. There are no situations in which the benefits of the medication to the mother outweigh the risks of harm to the baby. These medications should never be used by pregnant women.
Women who are able to become pregnant are recommended to use effective contraception during therapy, and for at some time after the last dose of Xgeva. Your doctor will tell you how long after your last dose you will have to use effective contraception.
Denosumab and Lactation
Tell your doctor if you are breastfeeding or plan to breastfeed.
It is not known if denosumab crosses into human milk. Because many medications can cross into human milk and because the possiblity for serious adverse reactions in nursing infants with use of this medication, a choice should be made whether to stop nursing or stop the use of this medication. Your doctor and you will decide if the benefits outweigh the risks of using denosumab.
Denosumab Usage
Take denosumab exactly as prescribed.
Denosumab comes as an injection and is given under the skin by a healthcare professional anywhere from once a month to every 6 months, depending on the condition being treated.
Denosumab Dosage
Take this medication exactly as prescribed by your doctor. Follow the directions on your prescription label carefully.
The dose your doctor recommends may be based on the following:
- the condition being treated
- other medical conditions you have
- other medications you are taking
- how you respond to this medication
The recommended dose of Prolia (denosumab) is 60 mg injected under the skin in the upper arm, upper thigh, or stomach every 6 months.
The recommended dose of Xgeva (denosumab) to:
- prevent fractures and treat those with multiple myeloma and those whose solid tumors have spread to the bone is 120 mg every 4 weeks.
- treat Giant Cell Tumor of Bone and high calcium levels due to cancer, the recommended dose of Xgeva (denosumab) is 120 mg every 4 weeks. An additional 120 mg will be injected on days 8 and 15 of the first month of treatment.
Xgeva (denosumab) is injected under the fatty layer of the skin (subcutaneous injection) in the upper arm, upper thigh, or stomach by a healthcare professional.
Denosumab Overdose
Since denosumab is administered by a healthcare provider in a medical setting, it is unlikely that an overdose will occur. However, if overdose is suspected, seek emergency medical attention.